Shaquille O’Neal, Davina McCall and other celebrities have been spotted wearing glucose monitors. Vogue just published two articles on blood sugar in a week - so it's a confirmed trend.
But why are people who don’t have diabetes suddenly wearing these little devices and why does blood glucose matter so much to them? The simplest reason - weight management.
Why would non-diabetics care about blood glucose levels?
It seems perfectly normal to have a heart monitor in your smart watch today, but many years ago, only sick people monitored their hearts continuously.
In 2024, monitoring blood glucose for weight loss and health will be reported as a big lifestyle trend. However, with big tech brands including Apple and Samsung working on integrating blood glucose monitoring into their devices, it’s not long until glucose monitoring becomes as normal as counting steps.
Why? Non-diabetics use blood glucose just as much as diabetics. Glucose fuels every cell in the body. However, diabetics have problems with storing excess glucose.
It’s useful to understand the difference between the two types of diabetes:
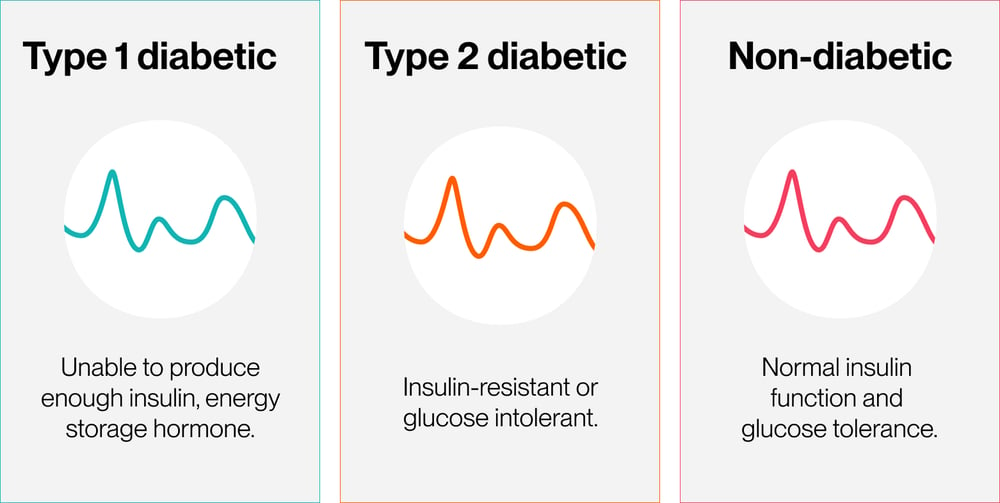
Type 1 diabetes: the pancreas can’t produce insulin, the energy storage hormone and the body can let too much sugar circulate in the blood, with fatal consequences.
Type 2 diabetes: brought about by diet and lifestyle over a period of time. The insulin mechanism gets worn out, the body becomes intolerant of glucose or both things happen.
The idea that non-diabetics should care about blood glucose levels isn’t new. For nearly 50 years, scientists have been racing to understand the growing prevalence of chronic degenerative diseases and worldwide decline in metabolic health. In the 80s, research into blood glucose led to the concept of ‘Glycaemic Index’(GI) which rates foods based on how quickly they raise blood sugar. It's since become a popular way of eating for health.
What's new about glucose monitoring: weight loss
Over time, we’ve come to understand the importance of energy regulation in overall health. And in the human body, energy regulation starts with blood glucose.
 The new wave of weight loss 'wonder drugs' were developed for diabetics
The new wave of weight loss 'wonder drugs' were developed for diabetics
Trendy weight loss drugs are all about blood glucose
There’s been a lot of media attention around blood glucose due to a new wave of weight loss drugs originally meant for type 2 diabetics.
These have gained traction after being used by celebrities and influencers for rapid weight loss. Injectables such as Semaglutide help the body lower blood glucose levels and regulate insulin, the hormone that helps the body store unused energy.
Elon Musk, Sharon Osbourne and Chelsea Handler have talked about how they've used the drug to change their weight.
While the drug works by interrupting hormonal processes that affect blood sugar, the effects wear off if the user doesn't make lasting habit changes. Yes, the weight comes back.
That's why some people are turning to monitoring instead, to make changes that last.
The Continuous Glucose Monitor
A better way to bring glucose under control
'Skinny jabs' became famous for the dramatic results and the speed at which they work. But the same changes can be brought about at the same rate without drugs. The trouble is, it requires data, knowledge and maybe most importantly, effort.
There's a growing trend of people without diabetes wearing continuous glucose monitors, with new start-ups offering various products and services.
As much as we want people to care deeply about their metabolic health, we find weight loss is the thing driving people to monitor their blood glucose.
Losing weight has a huge effect on a person's metabolic health, so that’s a good thing. As long as that monitoring is paired with knowledge.
Body fat starts as glucose
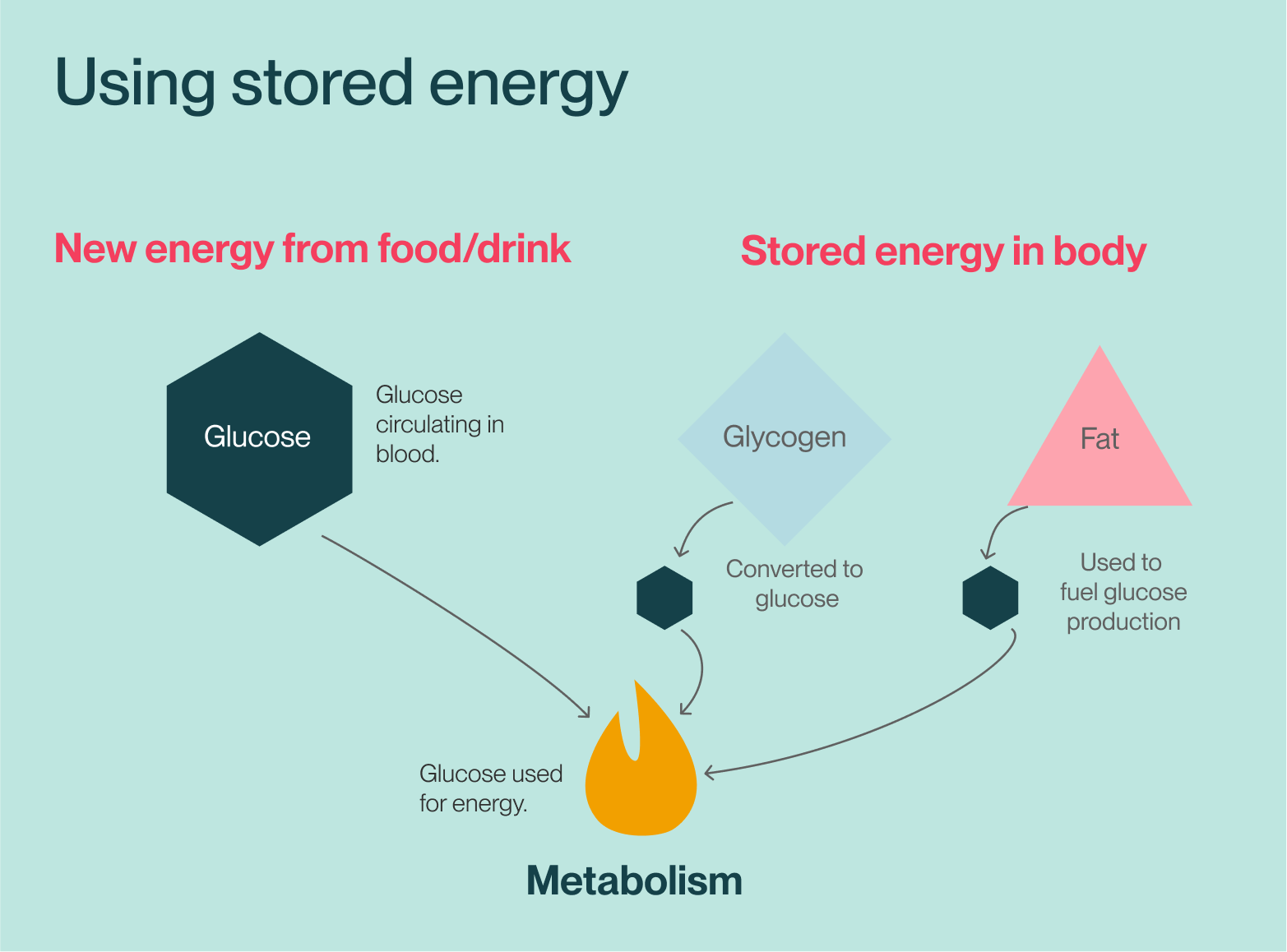
Understanding how your blood glucose can lead you to lose weight and you don’t need research to tell you that will improve your health. If you want to lose weight, you’re simply looking to use the energy your body stored because you didn't need it earlier - body fat.
Your body uses glucose to fuel everything it does and tightly regulates the amount of this fuel flowing round your system. The average human body keeps only a teaspoon of glucose in around 10 pints of blood.
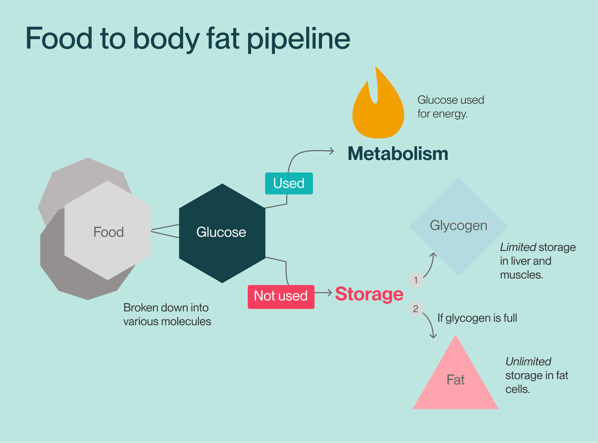
When you take in more than you need - which is ridiculously easy to do - your body needs to store the excess. If you’re not diabetic, your pancreas releases insulin to guide the glucose to your storage mechanisms:
- Glycogen. Glucose gets converted and stored in the liver and muscles. This is limited storage, with around 400g in the body.
- Fat. If the first store is full, excess energy is converted to fat and stored in fat cells. This is unlimited storage.
Stored fat is supposed to be used
The creation and storage of fat is a survival mechanism designed to protect you when there’s no energy around. That’s why most of us are so good at it. After your body's stored fat, it really wants to use it up.
It was a crucial function in the stone age, when you might not find food for days and the nearest supermarket was several thousands of years away.
That same mechanism has been sent haywire by the modern lifestyle. The fact that we carry excess energy around instead of using it stresses the body. For an increasing number of us, that mechanism is making us ill instead of keeping us well.
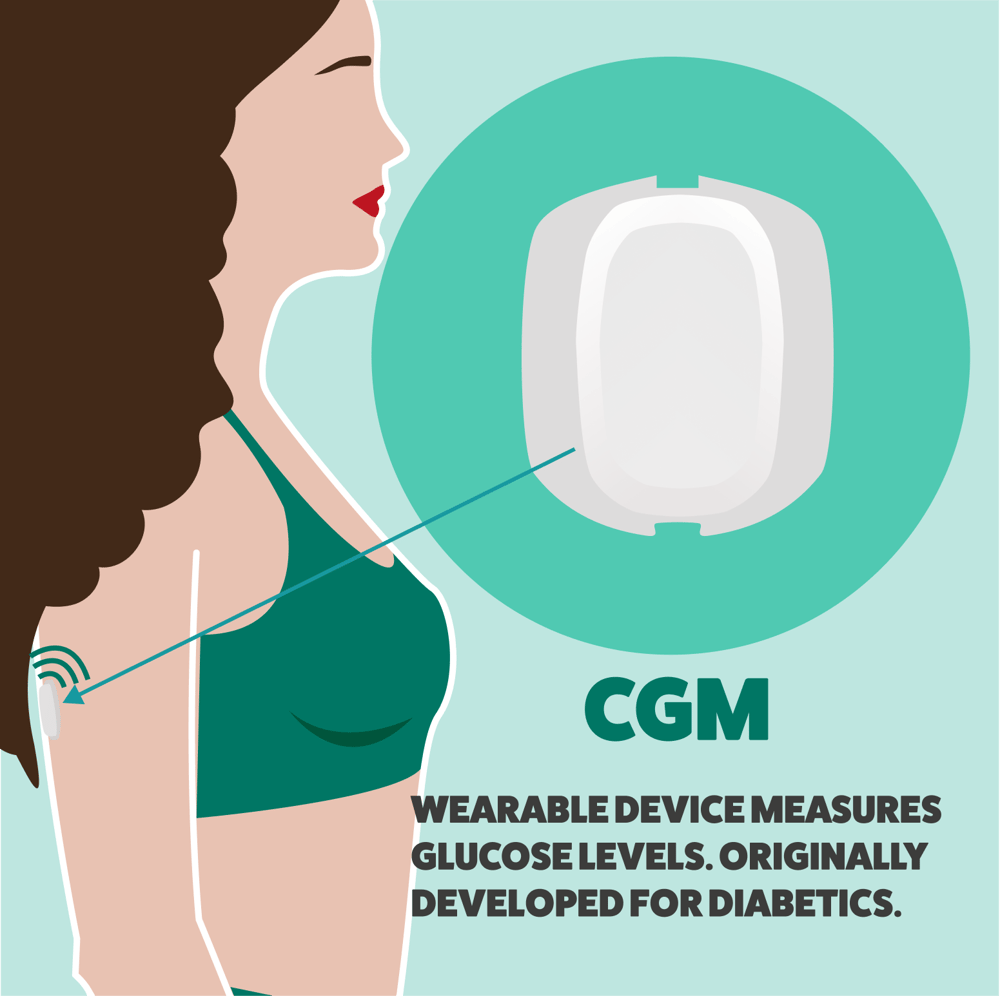
The continuous glucose monitor - CGM was originally developed for diabetics to tell them when to administer insulin because their pancreas either doesn’t make any or makes very little.
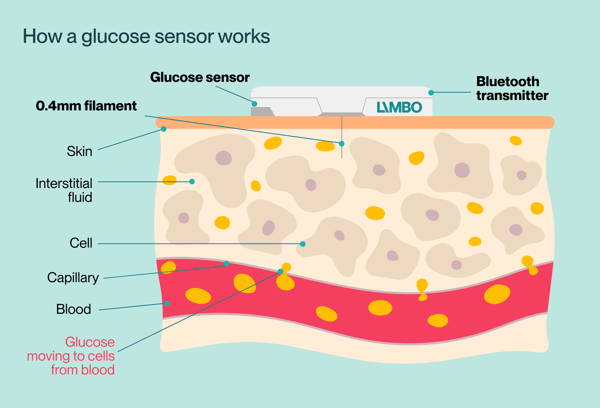
The wearable such as the Limbo sensor is stuck to the skin and estimates your blood sugar level using a filament inside your skin. Rather than sitting in your blood, the device measures glucose in your interstitial fluid.
As glucose is circulated to every cell in your body, using this fluid provides a reliable reading that matches what’s in your blood. Some CGMs take readings more often than others, so you don’t necessarily get a ‘live’ view of your blood glucose but close enough if you’re not managing diabetes.
How do you monitor blood glucose without a fancy CGM?
The alternative is to use finger-prick tests which are uncomfortable, inconvenient and can often lead to infections. Unfortunately, many diabetics still have to do this because CGMs are not cheap. But as more CGM companies enter the global market, prices for these devices will start to fall.
There’s no reliable non-invasive way to monitor glucose yet. But several technology companies are working on various solutions to this problem.
What CGM wearers see
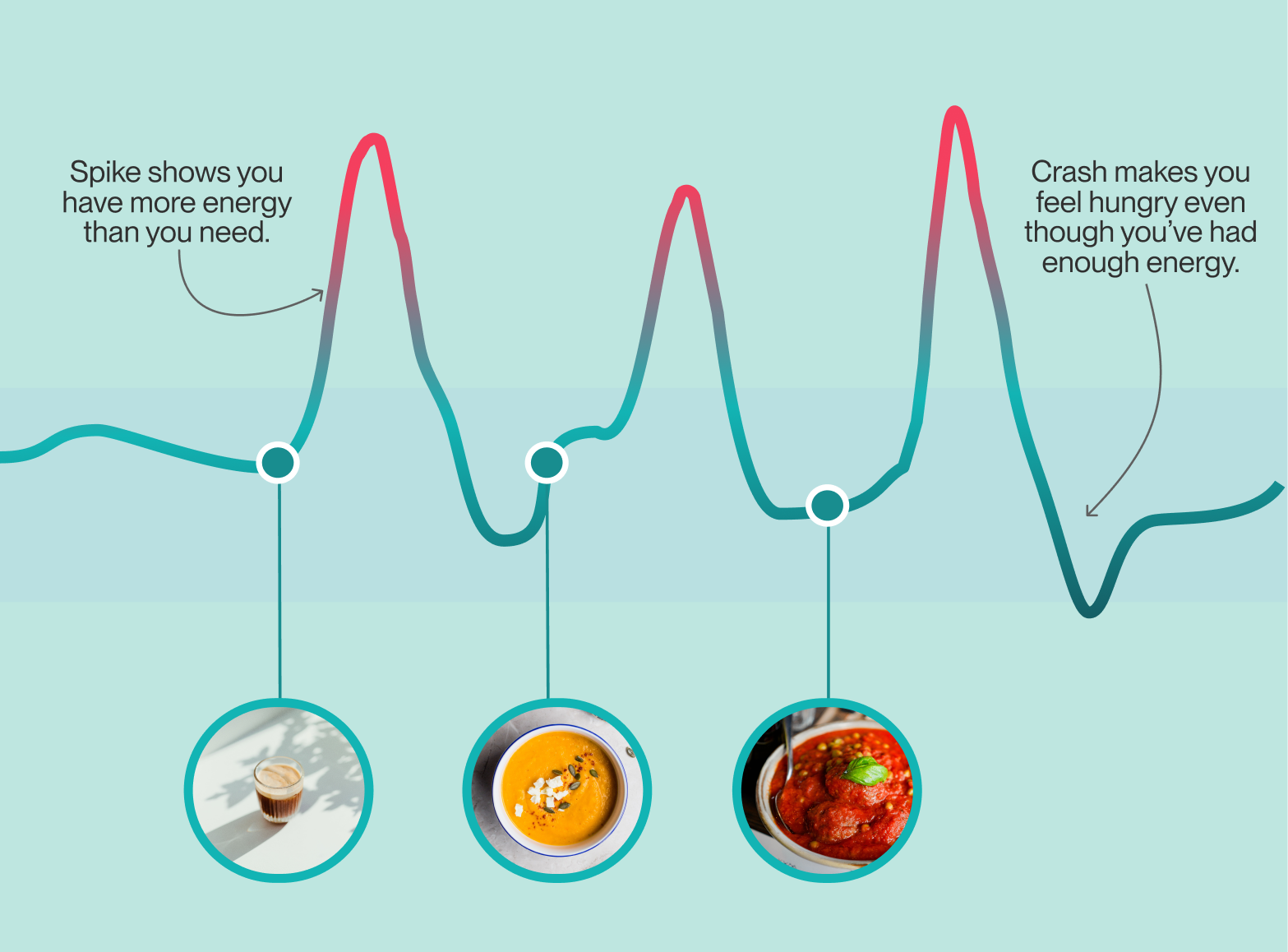
Your blood sugar rises and falls naturally throughout the day as your body takes in and uses energy. What CGM wearers quickly learn is that eating certain foods and doing certain things causes rises in their blood glucose and is sometimes followed by steep drops.
People wearing CGMs see what happens to their metabolism after they’ve done something like eat or exercise.
These are nothing to be alarmed about - they’re a natural function. But they are stressors. Over time, you can wear out the system your body uses to deal with excess glucose in your system. That’s how frequent spikes and crashes can eventually lead to type 2 diabetes.
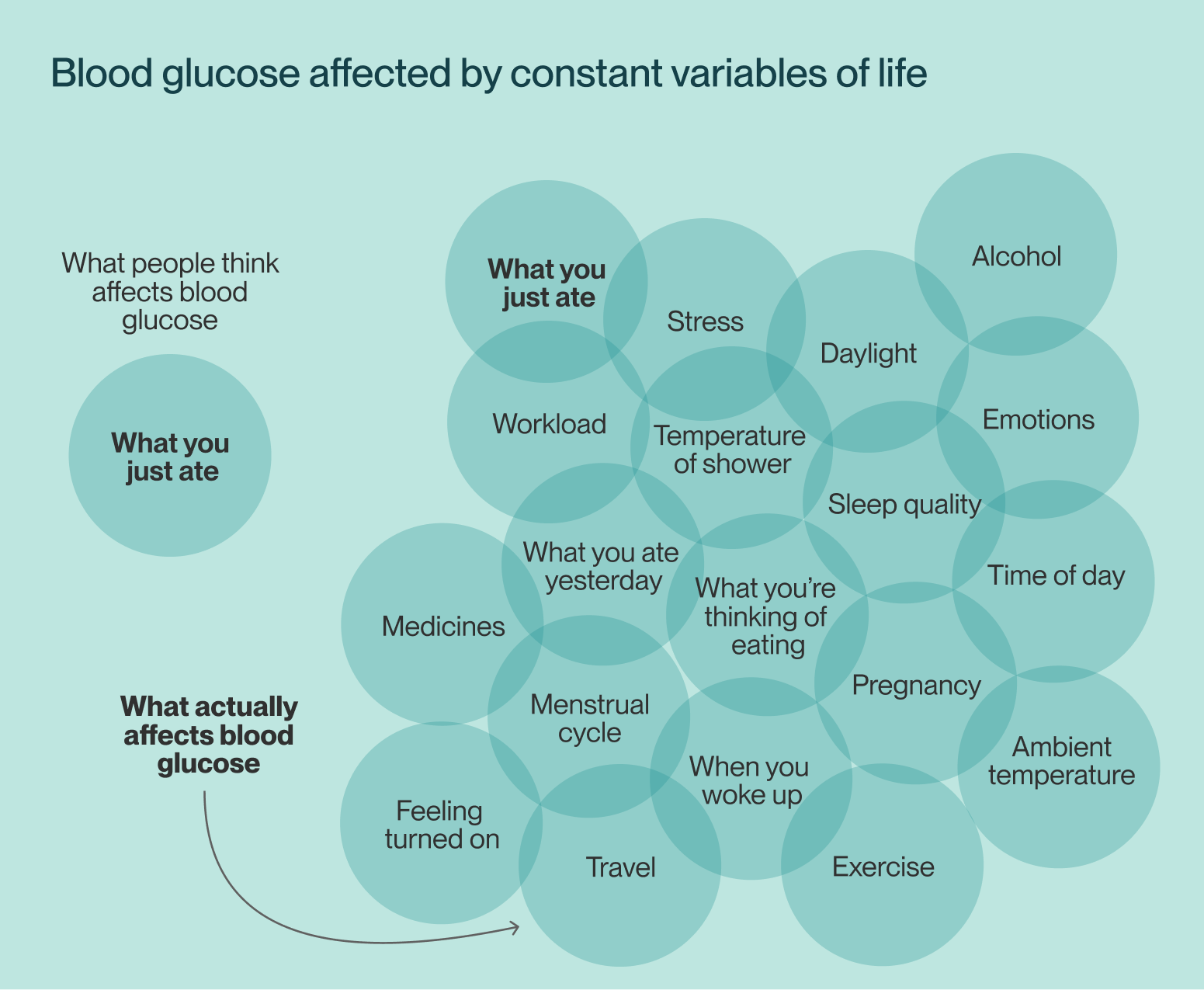
Blood glucose is affected by many constant variables
Constants and variables are usually opposites in science, but one thing living organisms are guaranteed is those variables are constantly changing.
Blood glucose levels are not just affected by food, drink and exercise. They can be affected by your mood, the ambient temperature and more.
Glucose is powering more than 37 trillion individual cells that make up your body. They're always in flux, so your blood glucose response will vary day to day.
That means you can react differently to the same food on different days.
Should I wear a CGM?
Understanding the impact your everyday choices have on your blood glucose can lead you to rapidly change your habits and improve the state of your metabolism.
On the other hand, continuous monitoring can also cause unnecessary worry, if you don’t understand what the data is telling you. Observing spikes and crashes without understanding what they mean can lead to unnecessary anxiety, incorrect self-diagnosis and bad decisions about food.
Life’s constant variables mean that a couple of weeks of monitoring (the average life of a sensor) won’t tell you how you’ll always respond to foods. And if you’re going through the process of changing the way you eat, your metabolism changes too - the way you respond to glucose changes!
So if you’re thinking of getting one of these trendy accessories, you have to consider whether you’ve got the right knowledge to make the right changes. Monitoring is pointless without the understanding to make meaningful changes.
But if you have the right advice, you’ll find the answer to sustainable weight loss has been inside you all the time.
See how Limbo uses CGMs and coaching in its revolutionary weight loss programme.
